Anal Fissure
Introduction
An anal fissure is a tear or ulcer (open sore) that develops in the lining of the anal canal.
The most common symptoms of anal fissures include:
- A sharp pain or burning sensation when passing a stool (poo)
- Noticing bright red blood on toilet paper or on the toilet seat
The anal canal
The anal canal is the last part of the large intestine (colon), and is located between the rectum (a small pouch where stools are stored) and the anus (the opening through which stools are passed out of the body).
The anal canal is approximately 2.5-4cm (1-1.5in) long in adults and is lined by a thin layer of cells known as squamous epithelium cells. If this lining becomes damaged, an anal fissure can develop.
Causes of anal fissures
Most anal fissures occur when passing particularly hard stools (constipation) which can damage the anal canal.
Other known causes include:
- Childbirth
- Persistent diarrhoea
- Inflammatory bowel disease (IBD), which is a general term for conditions that cause inflammation of the intestines, such as ulcerative colitis and Crohn’s disease
Anal fissures can also be classified according to how long symptoms last. For example:
- Acute anal fissure – where symptoms do not last longer than six weeks
- Chronic anal fissure – where symptoms last longer than six weeks
Treating anal fissures
Anal fissures usually heal within a few weeks without the need for medical treatment. Switching to a high-fibre diet should also help to relieve symptoms and speed up the recovery time because the fibre makes it easier to pass stools.
Treatment for chronic anal fissures can vary from person to person. Some cases can be relieved by switching to a high-fibre diet, whereas others may need medication or even surgery.
It is not always possible to prevent anal fissures, but you can take steps to prevent constipation, which is a common cause. This includes eating a healthy diet with plenty of fibre and drinking regular fluids.
Who is affected
Acute anal fissures are relatively common. They affect both sexes equally and occur in people of all ages, including children. However, younger adults between the ages of 20 to 40 are most likely to develop one. Chronic anal fissures are less common than acute anal fissures, but they are certainly not rare.
Symptoms of anal fissure
The symptoms of an anal fissure usually include pain and bleeding.
Pain
An anal fissure causes a severe and sharp pain when you pass stools (poo). Some people have described the pain as feeling like trying to pass broken glass. Once this sharp pain has passed, it is usually replaced by a deep burning pain, which may be felt for several hours after you have been to the toilet.
Bleeding
Anal fissures can also cause bleeding when you pass stools. Most people notice a small amount of bright red blood, either in their stools or on the toilet paper.
When to see Dr. B C Shah
Speak to Dr. B C Shah if you suspect that you have an anal fissure.
Most anal fissures get better without treatment, but Dr. B C Shah will want to rule out other conditions, such as haemorrhoids (swollen blood vessels in the anus and rectum).
They may also recommend treating the possible cause, such as dietary advice for constipation.
Causes of anal fissure
Anal fissures are most commonly caused by damage to the anus or the anal canal. Most cases first develop when a particularly hard or large stool damages the anal canal.
The main causes of anal fissures include:
- Constipation – which can cause people to strain when passing a stool
- Diarrhoea – particularly reoccurring (chronic) diarrhoea
- Inflammatory bowel disease (IBD) – such as Crohn’s disease and ulcerative colitis
- Pregnancy – your risk of developing an anal fissure is increased during the third trimester of pregnancy (from week 29 to birth)
- Childbirth – the continual straining of your muscles during childbirth can cause the lining of your anus to tear
- A sexually transmitted infection (STI) – if the lining of the anus becomes infected it can cause the tissue to break down, leading to an anal fissure
STIs known to affect the anus include:
- Syphilis – a bacterial infection that causes a wide range of symptoms
- Human papilloma virus (HPV) – the virus that causesgenital warts
- Herpes – a viral infection that can cause blistering around the genitals
- Chlamydia – a bacterial infection that can cause pain when passing urine but often shows no symptoms
Cancer of the anus
In very rare cases, an anal fissure can be a sign of cancer. Dr. B C Shah will be able to tell if your fissure is a sign of a more serious illness from your symptoms and the appearance of your fissure. They will refer you for further testing if they think it is necessary. It is important to remember that in the majority of cases, anal fissures are not caused by cancer.
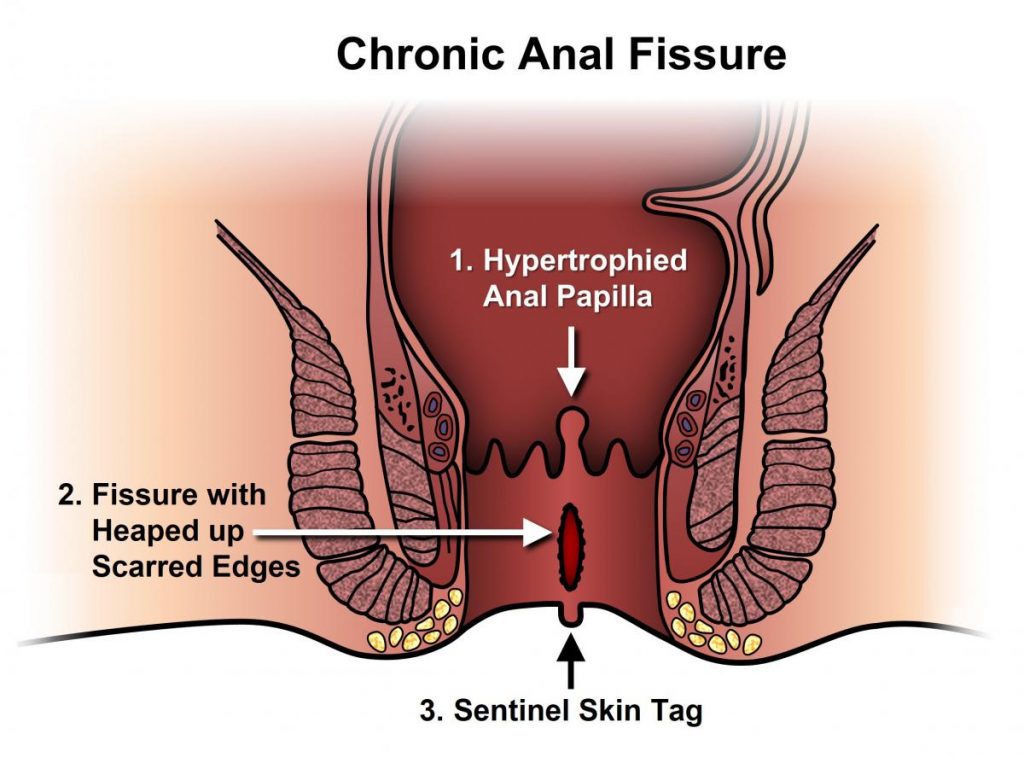
Chronic anal fissures
Some people may have underlying problems with the ring of muscle that surrounds their anal canal, known as the internal sphincter. These problems can prevent the anal canal from healing in the normal way, leading to the development of chronic anal fissures.
It is thought that some people have a sphincter muscle that is larger than normal, which produces muscle tension stronger than normal. The increased muscle tension causes increased pressure in the anal canal, making it more susceptible to tearing.
The increased pressure in the anal canal also restricts the blood flow to the anus. Reduced blood flow prevents your body from being able to heal itself as well as it usually can, making it difficult for your fissure to heal naturally. Furthermore, each time that you pass a stool, the injured tissue inside the anal canal is further damaged. This may be why some people develop chronic anal fissures.
Another common problem is that some people try to avoid passing stools due to the pain of an anal fissure. This can trigger the symptoms of constipation, which means that the fissure will not have a chance to heal.
Diagnosing anal fissure
To diagnose an anal fissure, Dr. B C Shah will first ask about your symptoms and the type of pain you have been experiencing. They may also ask about your toilet habits.
Physical examination
Dr. B C Shah will usually need to carry out a physical examination to confirm that you have an anal fissure. In most cases, he will be able to see the fissure by gently parting your buttocks.
If Dr. B C Shah cannot see a fissure, he may press gently on the edge of your anus. If you have an anal fissure, you will usually experience some pain when gentle pressure is applied.
Very rarely, Dr. B C Shah may need to perform a digital rectal examination (where he will insert a lubricated, gloved finger into your anus to feel for abnormalities) to diagnose an anal fissure.
Treating anal fissure
Like other small cuts or tears to the skin, an anal fissure will often heal by itself within a few weeks.
However, you may require treatment to help ease the pain and discomfort that an anal fissure can cause.
You should see Dr. B C Shah if you have the signs and symptoms of an anal fissure because it may be caused by an underlying condition. If this is the case and the condition is not treated, the fissure may not be able to heal and the problem will reoccur.
There are a number of treatments that encourage your anal fissure to heal, as well as easing your pain. These are described below.
Softening stools
Soft stools are easier to pass with less pain and discomfort, so Dr. B C Shah may recommend ways to soften your stools (outlined below).
Laxatives
Laxatives are a type of medicine that can help soften your stools.
Adults with an anal fissure will usually be prescribed a bulk-forming laxative. Bulk-forming laxatives work by helping your stools to retain fluid, making them softer and denser.
Children with an anal fissure are usually prescribed an osmotic laxative. This works by increasing the amount of fluid in your bowels, which stimulates your body to pass stools.
Once you start taking a laxative, Dr. B C Shah may have to adjust the dose until you find that your stools are soft and easy to pass.
Fibre
As well as using laxatives, you should also increase the amount of fibre in your diet. Foods high in fibre include:
- Wholegrain bread
- Brown rice
- Oats
- Beans
- Grains
- Seeds
- Fruit and dried fruit
- Vegetables
Adults should aim to eat at least 18g of fibre a day. You can see how much fibre a food item contains by looking at the nutritional information on the back of the packet.
If you are increasing your fibre intake, you should do so gradually. A sudden increase can cause stomach cramps and make you produce more wind, leaving you feeling bloated. It is also important to make sure that you drink plenty of water. You should aim to drink approximately 1.2 litres (six to eight glasses) of water a day, or more when you are exercising or when it is hot.
Baby wipes or toilet paper
It is important to avoid causing pain or irritation when wiping after passing a stool.
If you use baby wipes, do not use products that contain fragrance or alcohol as this could lead discomfort or itching. If you use toilet paper, use a soft brand if possible and avoid rubbing the area too hard.
Medications
Topical anaesthetics
A topical medicine is one that you apply directly to the affected area. Topical anaesthetics work by desensitising (numbing) the skin, which in the case of an anal fissure, will help ease the sharp and severe pain you may experience when passing stools.
Lidocaine is the most commonly prescribed topical anaesthetic. It either comes in the form of a gel or an ointment. Lidocaine is usually only used for one to two weeks because the fissure should start to heal within this time. It is usually applied shortly before passing a stool, but you should always follow the instructions that come with the medicine.
Painkillers
If you experience prolonged, burning pain after passing stools, you may be prescribed an analgesic (painkiller) such as paracetamol or ibuprofen. Again, you should always follow the dosage instructions on the patient information leaflet or packet.
Glyceryl trinitrate (GTN)
If your symptoms do not start to improve after a week, you may be prescribed a medicine called glyceryl trinitrate (GTN). GTN works by expanding nearby blood vessels, which helps to increase the blood supply to the site of the fissure. The increase in blood supply should enable the fissure heal more quickly.
GTN also reduces anal pressure. This should help reduce the pain. It comes in the form of an ointment and is applied directly to the anal area, usually every 12 hours.
GTN is not suitable for use by pregnant or breastfeeding women. It is also unsuitable for children. Headaches are a very common side effect of this type of medicine. Approximately 50% of people using GTN will experience a headache. Some people may also feel dizzy or light-headed after using GTN.
You will usually have to use GTN ointment for six to eight weeks, or until your fissure has completely healed.
Calcium channel blockers
Calcium channel blockers are a type of medication usually used to treat high blood pressure (hypertension). However, they have also proved useful in treating cases of anal fissures in some people.
Topical calcium channel blockers work by relaxing the sphincter muscle and increasing the blood supply to the site of the fissure.
Side effects of topical calcium channel blockers may include:
- Headache
- Dizziness, particularly when standing up from a sitting or lying position
- Itchiness or burning at the site when you apply the medication
However, the side effects caused by calcium channel blockers should pass within a few days once your body gets used to the medication.
There is no evidence that calcium channel blockers are more effective than GTN, so they tend only to be used in people unable or unwilling to take GTN.
Botulinum toxin
Botulinum toxin is a relatively new treatment for anal fissures. It’s usually used if other treatments have failed.
Botulinum toxin is a powerful poison which is safe to use in small doses. In cases of anal fissure, an injection of the toxin can be used to paralyse your sphincter muscle. This should prevent the muscle from spasming (contracting), helping to reduce pain and allowing the fissure to heal.
Botulinum toxin is an effective treatment in the short to medium term, with three out of four people remaining symptom-free for six months after treatment. Further treatment may be required in the long-term, as around half of people experience a return of their symptoms within three years.
Follow-up
Dr. B C Shah will usually arrange for you to have a follow-up appointment, approximately eight weeks after the start of your treatment. This will enable him to check that your fissure has healed, or is showing adequate signs of improvement.
If your condition has not been completely treated, Dr. B C Shah may recommend a further follow-up appointment six to eight weeks later.
If your anal fissure is particularly severe, or does not respond to treatment after eight weeks, you may have specialist treatment. This will usually involve having some type of surgery.
Surgery
There are a number of different surgical techniques that can be used to treat an anal fissure. These are discussed below.
Internal sphincterotomy
An internal sphincterotomy involves removing a section of the sphincter muscle. This helps to reduce the tension in the muscle, preventing further spasms of the sphincter and allowing the anal fissure to heal.
An internal sphincterotomy is a relatively straightforward operation that can be performed using a local anaesthetic on a day patient basis, which means you will not have to spend the night in hospital.
An internal sphincterotomy is an effective treatment with a good track record of success. People who have this type of surgery will experience healing of their anal fissure.
Some people will experience bowel incontinence after having surgery due to damage to the anal muscles. This means they will lose some control of their bowel movements. However, it is usually a mild type of incontinence where the person is unable to prevent themselves from passing wind, and they may also experience some mild soiling.
The symptoms of incontinence usually improve in the first few months after surgery and resolve within two months. However, in some cases the incontinence is permanent.
Fissurectomy
A fissurectomy is the surgical removal of an anal fissure, along with the surrounding tissue.
Fissurectomies are not as widely used as internal sphincterotomies because they do not treat the underlying causes. Therefore, a fissurectomy may not prevent anal fissures from reoccurring in the future.
However, a fissurectomy may be a recommended treatment option for children because removing a section of the sphincter muscle at an early age could cause permanent incontinence.
Advancement anal flaps
Advancement anal flaps involve taking healthy tissue from another part of your body and using it to repair the fissure and improve the blood supply to the site of the fissure.
This is often recommended to treat cases of chronic anal fissure, which have occurred as a result of pregnancy or other injury to the anus.
Preventing anal fissure
It is not always possible to prevent an anal fissure. However, one of the best ways to prevent one from developing is to avoid becoming constipated.
The best ways to prevent constipation are outlined below.
Fibre
Make sure you have enough fibre in your diet. Most adults do not eat enough fibre. You should have approximately 18g of fibre a day. You can increase your fibre intake by eating more of these foods:
- Fruit
- Vegetables
- Wholegrain rice
- Wholewheat pasta
- Wholemeal bread
- Seeds
- Nuts
- Oats
Eating more fibre will keep your bowel movements regular because it helps food pass through your digestive system more easily. Foods high in fibre also make you feel fuller for longer.
If you are increasing your fibre intake, it is important to increase it gradually. A sudden increase may make you feel bloated. You may also produce more flatulence (wind) and have stomach cramps.
Fluids
Make sure you drink plenty of fluids to avoid dehydration and steadily increase your intake when you are exercising or when it is hot. Try to cut back on the amount of caffeine, alcohol and fizzy drinks you consume.
Toilet habits
Never ignore the urge to go to the toilet. Ignoring the urge can significantly increase your chances of having constipation. The best time for you to pass stools is first thing in the morning, or about 30 minutes after a meal.
When you use the toilet, make sure you have enough time and privacy to pass stools comfortably.
Exercise
Keeping mobile and active will greatly reduce your risk of getting constipation. Ideally, do at least 150 minutes of physical activity every week.
Not only will regular exercise reduce your risk of becoming constipated, but it will also leave you feeling healthier and improve your mood, energy levels and general fitness.
 Dr. Bimal Shah is the senior most General & Laparoscopic surgeon in Mira – Bhayandar with largest series of operations. He also consults at Borivali – Dahisar. He believes in ethical practice & is available at only trust hospitals. He passed out from KEM hospital, Mumbai in 1993 and was a lecturer training newer surgeons & medical students till 1998.
Dr. Bimal Shah is the senior most General & Laparoscopic surgeon in Mira – Bhayandar with largest series of operations. He also consults at Borivali – Dahisar. He believes in ethical practice & is available at only trust hospitals. He passed out from KEM hospital, Mumbai in 1993 and was a lecturer training newer surgeons & medical students till 1998. 






